Which Agents of Bioterrorism Can Be Treated Effectively With Antibiotics? Select All That Apply.
From a scientific and medical perspective, bioterrorism—using biological weapons to produce affliction in humans—can be viewed as a variation of the problem of emerging infectious diseases, the only departure being that increased virulence or intentional release are deliberate acts. The U.s. public health organisation and main healthcare providers must exist prepared to address various biological agents, including pathogens that are rarely seen in this country.
Covert vs. Overt Bioterrorism
As with chemical agents, the intentional release of biological agents tin be either covert or overt. A covert release is unannounced and hidden, and may go unnoticed for days or even weeks. The presence of ill individuals may be the first sign of a release, and those infected may have inadvertently infected others. An infected person may seek medical intendance anywhere within the healthcare organization, mayhap at a distance from the release area.
An overt release is immediately credible and may even be appear. In an overt release, the healthcare arrangement and public health officials may be overwhelmed by requests for information and treatment. Hospitals, clinics, emergency responders, and advice systems volition be pressed into firsthand service. An overt release has the potential to cause widespread panic.
Whether the release is covert or overt, healthcare providers should be alert to illness patterns and diagnostic clues that signal an unusual communicable diseases outbreak that could be associated with intentional release of a biological amanuensis. In addition that should sentry for increases in unexpected or unexplained illnesses and know how to actuate the public health response system if an outbreak is suspected (CDC, 2001). Well-trained and educated first responders, showtime receivers, and public health personnel are essential to an organized and successful response.
Improving Response to Biologically Induced Illness
Healthcare providers, clinical laboratory personnel, infection command professionals, and public health departments play critical and complementary roles in the recognition and response to illness caused past the intentional release of biological agents. Syndrome descriptions, epidemiologic clues, and laboratory recommendations provide basic guidance that can improve recognition of these events (CDC, 2001).
Since 9/11, country and local health departments have initiated activities to meliorate recognition, reporting, and response, ranging from enhancing communications to conducting special surveillance projects. This includes agile tracking for changes in the number of hospital admissions, emergency department visits, and occurrence of specific syndromes. Bioterrorism preparedness activities and work with emerging infectious diseases accept helped public health agencies prepare for the intentional release of a biological amanuensis (CDC, 2001). The CDC's Emergency Preparedness and Response website has links to and data on the diverse tools available, as well as other resource.
Recognizing Clinical Syndromes
Work continues on syndromic surveillance projects and the CDC maintains electric current data on this enquiry. The term syndromic surveillance means watching for health-related data that signal sufficient probability of a case or an outbreak to warrant further public health response. Historically, syndromic surveillance was used in investigating potential cases, but its utility for detecting outbreaks associated with bioterrorism is increasingly being explored by public health officials. Technology changes and the plethora of programs and data have also affected these efforts (CDC, 2004b, 2012; Dembek, 2004). (Come across besides the CDC resource website).
The release of a biological agent may not have an firsthand impact because of the delay between exposure and onset of illness, and considering outbreaks associated with intentional releases may resemble naturally occurring ones. Nevertheless, healthcare workers should exist familiar with indications of intentional release of a biological agent and know when, and to whom, to study a suspected outbreak.
These indications include unusual clustering of disease, patients presenting with clinical signs and symptoms that suggest an infectious affliction outbreak, unusual age distribution for common diseases, and a large number of cases of acute flaccid paralysis with prominent bulbar palsies, which is suggestive of a release of botulinum toxin (CDC, 2001).
Epidemiologic Clues That May Signal a Covert Bioterrorism Attack
- Large number of sick persons with similar disease or syndrome.
- Large number of unexplained disease, syndrome or deaths.
- Unusual illness in a population.
- Higher morbidity and mortality than expected with a common affliction or syndrome.
- Failure of a common illness to respond to usual therapy.
- Unmarried case of disease caused past an uncommon amanuensis.
- Multiple unusual or unexplained disease entities circumstantial in the same patient without other explanation.
- Disease with an unusual geographic or seasonal distribution.
- Multiple atypical presentations of affliction agents.
- Similar genetic type among agents isolated from temporally or spatially distinct sources.
- Unusual, atypical, genetically engineered, or antiquated strain of agent.
- Endemic disease with unexplained increase in incidence.
- Simultaneous clusters of similar illness in non-face-to-face areas, domestic or foreign.
- Singular aerosol, food, or h2o transmission.
- Ill people presenting near the same time.
- Deaths or disease among animals that precedes or accompanies illness or expiry in humans.
- No disease in people not exposed to common ventilation systems, simply disease amongst those people in proximity to the systems (CDC, 2001a)
As noted earlier, a diverseness of factors affect the potential public health impact of an intentionally released biological agent:
- Lethality—how effectively information technology kills
- Infectivity—how easily it spreads
- Virulence—how likely it is to cause disease
- How easily is information technology dispersed
- Availability of medical handling and/or vaccine
- Dosage needed to cause illness
- Stability of the chemical compound (NTI, 2015a)
It may be difficult to pinpoint the time and location of a biological agent's release because of the variation in incubation catamenia among organisms. Some diseases evidence a rapid onset of symptoms and early treatment is critical. For example, plague has a rapid onset and is potentially fatal within 12 to 24 hours if untreated; botulism toxin also has a rapid onset and requires immediate supportive handling. On the other hand, smallpox tin exist treated effectively by vaccination within 2 to three days of symptom onset. Merely smallpox, like plague, is highly contagious and has the potential to crusade widespread panic, and in the case of smallpox, which is believed to have been eradicated, not enough vaccine exists should a widespread outbreak occur. Conversely, plague and anthrax, despite their potential for causing serious affliction and expiry, are finer treated with antibiotics.
Categories of Diseases and Biological Agents
Bioterrorism agents can be separated into three categories, depending on how easily they tin exist spread and the severity of illness or death they cause. Category A agents are considered the highest risk and Category C agents are those that are considered emerging threats for affliction (CDC, 2007).
Category A Diseases or Agents
Category A diseases or agents are high priority and include organisms that pose the highest risk to the public and national security considering they:
- Are easily spread or transmitted from person to person
- Result in high mortality rates and have the potential for major public health impact
- May cause public panic and social disruption
- Require special action for public health preparedness (CDC, 2007)
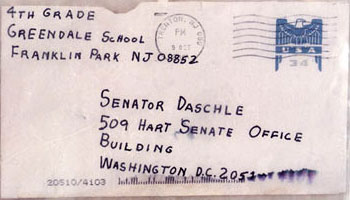
A alphabetic character sent in 2001 to Senate Majority Leader Tom Daschle contained anthrax pulverisation. Beginning one calendar week after the September 11 attacks, letters containing anthrax spores were mailed to several news media offices and 2 U.South. Senators, killing v people and infecting 17 others. Source: Wikimedia Commons.
Category A bioterrorism agents are:
- Anthrax
- Botulism
- Plague
- Smallpox
- Tularemia
- Viral hemorrhagic fevers (VHF) (CDC, 2013a)
Category B Diseases or Agents
Category B diseases or agents are the second highest priority because they:
- Are moderately easy to disseminate
- Result in moderate illness rates and low mortality rates
- Require specific enhancements of CDC's laboratory capacity and enhanced disease surveillance (CDC, 2007)
Category B diseases or agents include:
- Brucellosis (Brucella species)
- Epsilon toxin of Clostridium perfringens
- Food safety threats (Salmonella species, Escherichia coli O157:H7, and Shigella)
- Glanders (Burkholderia mallei)
- Melioidosis (Burkholderia pseudomallei)
- Psittacosis (Chlamydia psittaci)
- Q fever (Coxiella burnetii)
- Ricin toxin from Ricinus communis (castor beans)
- Staphylococcal enterotoxin B
- Typhus fever (Rickettsia prowazekii)
- Viral encephalitis (alphaviruses—Venezuelan equine encephalitis, eastern and western equine encephalitis)
- H2o safe threats (Vibrio cholerae, Cryptosporidium parvum) (CDC, 2008)
Category C Diseases or Agents
Category C diseases or agents are the third highest priority and include emerging pathogens that could be engineered for mass dissemination in the future considering:
- Are easily available
- Are hands produced and spread
- Take potential for high morbidity and mortality rates and major health impact (CDC, 2007)
Clinical Features of High-Priority Agents
4 category A diseases accept been the focus of the CDC's efforts to educate the healthcare community about bioterrorism potential: anthrax, botulism, plague, and smallpox. The CDC does not prioritize these agents in any order of importance or likelihood of use. Other agents with bioterrorism potential include those that crusade tularemia and viral hemorrhagic fevers (category A), brucellosis, Q fever, viral encephalitis, and illness associated with staphylococcal enterotoxin, category B. Other important category B agents include any organism that threatens the water or food supply.
Anthrax
Anthrax has been recognized equally an communicable diseases of animals and humans for millennia. Inside the U.s.a., animal anthrax is reported in nearly years, but naturally occurring human anthrax is rare. Worldwide, still, the illness is common in wild and domestic animals and not uncommon among persons who interact with animals in agricultural regions of South and Central America, sub-Saharan Africa, central and southwestern Asia, and southern and eastern Europe (Hendricks, et al. [CDC], 2014).
Bacillus anthracis, the causative agent of anthrax, is a nonmotile spore-forming, gram-positive, rod-shaped bacterium. Biodefense experts oft place B. anthracis at or most the top of the list for potential threat agents. Inhalation anthrax is particularly deadly, as demonstrated by the 1979 accidental release of B. anthracis from a military microbiology facility in the Sverdlovsk region of Russia; 88% (66/75) of patients reported with inhalation anthrax died. More recently, humans have caused disease from exposure to spores released purposefully as a bioterrorist weapon and accidentally from naturally occurring sources (Hendricks, et al. [CDC], 2014).
If a bioterrorist attack were to happen, Bacillus anthracis would be one of the biological agents nigh likely to exist used. Biological agents are germs that tin sicken or impale people, livestock, or crops. Anthrax is one of the near probable agents to be used considering:
- Anthrax spores are easily found in nature, can be produced in a lab, and tin can last for a long time in the environment.
- Anthrax makes a skilful weapon because it can be released quietly and without anyone knowing. The microscopic spores could be put into powders, sprays, food, and water. Because they are so minor, you lot may not be able to meet, scent, or taste them.
- Anthrax has been used as a weapon earlier. (CDC, 2014)
Anthrax has been used equally a weapon around the earth for nearly a century. In 2001, powdered anthrax spores were deliberately put into letters that were mailed through the U.S. postal organization. Twenty-two people, including 12 mail handlers, got anthrax, and five of these 22 people died.
A subset of select agents and toxins have been designated as Tier ane considering these biological agents and toxins present the greatest hazard of deliberate misuse with significant potential for mass casualties or devastating effect to the economy, critical infrastructure, or public confidence, and pose a severe threat to public health and rubber. Bacillus anthracis is a Tier ane agent.
An anthrax attack could take many forms. For case, it could exist placed in letters and mailed, as was done in 2001, or it could be put into food or water. Anthrax also could be released into the air from a truck, edifice, or plane. This type of attack would mean the anthrax spores could easily be diddled around past the wind or carried on people's wearing apparel, shoes, and other objects. It simply takes a small amount of anthrax to infect a large number of people.
If anthrax spores were released into the air, people could exhale them in and go sick with anthrax. Inhalation anthrax is the near serious form and can impale quickly if not treated immediately. If the assail were not detected by i of the monitoring systems in place in the United States, information technology might go unnoticed until doctors begin to come across unusual patterns of illness among sick people showing up at emergency rooms (CDC, 2014).
There are four clinical forms of anthrax: cutaneous or peel, respiratory tract or inhalation, gastrointestinal, and injection anthrax (has occurred in Europe simply not in the United states) (CDC, 2013b).
Cutaneous Anthrax
When anthrax spores get into the peel, usually through a cutting or scrape, a person tin develop cutaneous anthrax. This can happen when a person handles infected animals or contaminated animate being products like wool, hides, or hair. Cutaneous anthrax is nearly common on the head, neck, forearms, and hands. It affects the skin and tissue around the site of infection.
Cutaneous anthrax is the most common form of anthrax infection, and it is too considered to be the least dangerous. Infection usually develops from ane to 7 days afterwards exposure. Without treatment, upwardly to 20% of people with cutaneous anthrax may die. Even so, with proper treatment, almost all patients with cutaneous anthrax survive (CDC, 2013b).
Cutaneous anthrax symptoms can include:
- A grouping of small blisters or bumps that may itch
- A painless skin sore (ulcer) with a black heart that appears subsequently the small blisters or bumps
- Most often the sore will exist on the face, neck, arms, or hands
- Swelling can occur around the sore (CDC, 2013b)
Inhalation Anthrax
When a person breathes in anthrax spores, they tin develop inhalation anthrax. People who work in places such every bit wool mills, slaughterhouses, and tanneries may breathe in the spores when working with infected animals or contaminated animate being products from infected animals. Inhalation anthrax starts primarily in the lymph nodes in the chest earlier spreading throughout the rest of the trunk, ultimately causing astringent breathing problems and stupor.
Inhalation anthrax is considered to be the most deadly class of anthrax. Infection usually develops within a calendar week after exposure, but it can accept up to 2 months. Without treatment, only almost 10% to 15% of patients with inhalation anthrax survive. Still, with aggressive handling, about 55% of patients survive (CDC, 2013b).
Inhalation anthrax symptoms can include:
- Fever and chills
- Chest discomfort
- Shortness of breath
- Confusion or dizziness
- Coughing
- Nausea, vomiting, or tum pains
- Headache
- Sweats (often drenching)
- Extreme tiredness
- Torso aches (CDC, 2013b)
Gastrointestinal Anthrax
When a person eats raw or undercooked meat from an animal infected with anthrax, they can develop gastrointestinal anthrax. Once ingested, anthrax spores can affect the upper gastrointestinal tract (throat and esophagus), stomach, and intestines.
Gastrointestinal anthrax has rarely been reported in the United States. Infection normally develops from 1 to seven days afterwards exposure. Without treatment, more than half of patients with gastrointestinal anthrax die. Still, with proper treatment, threescore% of patients survive (CDC, 2013b).
Gastrointestinal anthrax symptoms can include:
- Fever and chills
- Swelling of cervix or neck glands
- Sore pharynx
- Painful swallowing
- Hoarseness
- Nausea and airsickness, especially bloody vomiting
- Diarrhea or bloody diarrhea
- Headache
- Flushing (cerise face up) and ruby eyes
- Stomach pain
- Fainting
- Swelling of abdomen (stomach) (CDC, 2013b)
Injection Anthrax
Recently, another type of anthrax infection has been identified in heroin-injecting drug users in northern Europe. This blazon of infection has never been reported in the United States.
Symptoms may exist similar to those of cutaneous anthrax, just there may be infection deep under the peel or in the muscle where the drug was injected. Injection anthrax can spread throughout the trunk faster and be harder to recognize and treat. Lots of other more common bacteria can cause skin and injection site infections, so a skin or injection site infection in a drug user does not necessarily hateful the person has anthrax (CDC, 2013b).
Injection anthrax symptoms tin can include:
- Fever and chills
- A group of small blisters or bumps that may crawling, appearing where the drug was injected
- A painless skin sore with a black center that appears after the blisters or bumps
- Swelling around the sore
- Abscesses deep under the skin or in the muscle where the drug was injected
- Continue in mind
- Symptoms are similar to those of cutaneous anthrax, just injection anthrax tin can spread throughout the torso faster and be harder to recognize and treat than cutaneous anthrax.
- Skin and injection site infections associated with injection drug use are mutual and do not necessarily hateful the person has anthrax. (CDC, 2013b)
Botulism
Botulism is a neuroparalytic (muscle-paralyzing) illness whose agent is the toxin produced by Clostridium botulinum—an encapsulated, anaerobe, gram-positive, spore-forming, rod-shaped bacterium (CDC, 2006). Botulism neurotoxin is an extremely strong organism; less than 1 microgram causes fatality in adults. It causes paralysis past inhibiting the release of acetylcholine at the neuromuscular junction; respiratory paralysis and death result if left untreated. In that location are four forms of naturally occurring botulism:
Foodborne Botulism
- Caused by ingestion of pre-formed toxin
Infant Botulism
- Caused by ingestion of C. botulinum, which produces toxin in the intestinal tract
Wound Botulism
- Acquired by wound infection with C. botulinum that secretes the toxin
Adult Intestinal Colonization
- Rare, caused when C. botulinum colonizes the abdominal tract of children or adults, usually with gastrointestinal abnormalities (CDC, 2006)
Botulinum toxin as a biological weapon
- Aerosolized botulinum toxin is a possible mechanism for a bioterrorism assail
- Inhalational botulism does non occur naturally
- Inhalational botulism cannot be clinically differentiated from the three naturally occurring forms
- Indications of intentional release of a biologic agent may include:
- An unusual geographic clustering of illness (eg, persons who attended the same public event or gathering)
- A large number of cases of acute flaccid paralysis with prominent bulbar palsies, especially if occurring in otherwise salubrious persons (CDC, 2006)
Botulism is non transmissible from person to person. For foodborne botulism, symptoms begin within 6 hours to ten days after exposure (often within 12–36 hours), and could be shorter in inhalational botulism (CDC, 2006b).
| Symptoms, Diagnosis, and Handling of Botulism | |
|---|---|
| Symptoms/ |
|
| Diagnosis/ |
|
| Treatment |
|
| Prophylaxis |
|
Plague (Yersinia pestis)
Plague is an acute and potentially fatal bacterial infection that affects humans and animals and is acquired past Y. pestis. Plague usually presents as i of 5 master clinical syndromes: bubonic, pneumonic, septicemic, plague meningitis, or pharyngeal. Plague is a naturally occurring illness that has been endemic in the United States since 1900. Approximately 5 to fifteen cases occur per year, with the greatest concentration of cases in Arizona, Colorado, and New United mexican states (CDC, 2004a).
An immediate and coordinated public health and medical response would exist required in the event of the intentional employ of plague. Therefore, whatsoever instance of plague should be reported to the state health department immediately. Reporting is especially important when a case of plague occurs outside of a typically affected area (CDC, 2004a).
With bubonic plague, the infection is transmitted past the bite of an infected flea or exposure to infected material through a break in the pare. Bubonic plague cannot be transmitted from person to person. If bubonic plague is not treated, the bacteria can spread through the bloodstream and infect the lungs, causing a secondary infection of pneumonic or septicemic plague (CDC, 2004a).
Pneumonic plague is a pulmonary infection that occurs upon inhalation of plague bacteria. Pneumonic plague can be transmitted person to person through respiratory droplets with direct close contact, and without early treatment in less than 24 hours, pneumonic plague about universally leads to respiratory failure, shock, and rapid decease (CDC, 2004a).
Infection via inhalation of infective respiratory droplets or aerosols is rare with naturally occurring plague in the U.s., but is the most probable road of transmission in a bioterrorist event. If Y. pestis were to exist used as a bioweapon, information technology would be most dangerous if released every bit an aerosol. An aerosol release would be expected to consequence in an outbreak of the pneumonic form of plague and it may too cause the less common pharyngeal plague and ocular plague (CDC, 2004a).
The chief form of septicemic plague results from straight inoculation and multiplication of plague bacilli in the bloodstream, while the secondary form is a evolution of untreated pneumonic or bubonic plague (CDC, 2004a).
Bubonic Plague
- Incubation menses: 2 to 6 days
- Symptoms
- Lymphadenopathy and fever are both early on symptoms of bubonic plague.
- Patients develop buboes, which are grossly enlarged, extremely tender lymph nodes draining at the corresponding site of inoculation.
- Progression of disease: If bubonic plague is not treated, the leaner tin can spread through the bloodstream, causing septicemia, or it can infect the lungs, causing a secondary case of pneumonic plague. Rarely, it can progress to meningitis. (CDC, 2004a)
Pneumonic Plague
- Incubation period: ii to 4 days with range of ane to 6 days
- Symptoms
- Acute onset of fever, chills, malaise, and myalgias associated with progressive lethargy
- A productive cough of copious watery mucoid sputum that may exist bloody
- Associated breast pain and increasing dyspnea
- Progression of affliction: As the disease progresses, adult respiratory distress syndrome (ARDS) characterized by refractory pulmonary edema may occur. Signs of daze, including hypotension and eventual multi-organ failure, may also occur. Without early detection and treatment in less than 24 hours, pneumonic plague is almost universally fatal. (CDC, 2004a)
Septicemic Plague
- Incubation menses: Occurs when plague bacteria multiply in the blood. Most commonly, septicemic plague presents as a complexity of pneumonic or bubonic plague, but primary septicemic plague can occur.
- Symptoms: Astute onset of fever, chills, prostration, abdominal pain, nausea, and vomiting.
- Progression of disease: As the affliction progresses, purpura may develop, as well as possible disseminated intravascular coagulation (DIC). Eventually, hypotension and other signs of stupor announced. Septicemic plague is often fatal even when treated. (CDC, 2004a)
Smallpox (Variola)
Smallpox is a serious, contagious, and sometimes fatal communicable diseases. At that place is no specific handling for smallpox disease, and the only prevention is vaccination. The pox function of smallpox is derived from the Latin discussion for "spotted" and refers to the raised bumps that appear on the confront and body of an infected person (CDC, 2004c).
There are 2 clinical forms of smallpox. Variola major is the severe and well-nigh mutual grade of smallpox, with a more extensive rash and college fever. In that location are four types of variola major smallpox: ordinary (the nigh frequent type, accounting for 90% or more of cases); modified (mild and occurring in previously vaccinated persons); flat; and hemorrhagic (both rare and very severe). Historically, variola major has an overall fatality rate of almost xxx%; even so, flat and hemorrhagic smallpox commonly are fatal. Variola minor is a less common presentation of smallpox, and a much less severe disease, with expiry rates historically of 1% or less (CDC, 2004c).
Smallpox is caused by the variola virus, which emerged in human populations thousands of years ago, but the disease is now eradicated after a successful worldwide vaccination plan. After the disease was eliminated from the earth, routine vaccination against smallpox among the full general public was stopped because it was no longer necessary for prevention. Except for laboratory stockpiles, the variola virus has been eliminated. However, in the aftermath of nine/xi, in that location is heightened concern that the variola virus might be used as an agent of bioterrorism. For this reason, the U.S. authorities is taking precautions for dealing with a smallpox outbreak (CDC, 2004c).
Mostly, direct and fairly prolonged confront-to-face contact is required to spread smallpox from one person to another. Smallpox besides tin exist spread through direct contact with infected actual fluids or contaminated objects such as bedding or clothing. Rarely, smallpox has been spread past virus carried in the air in enclosed settings such equally buildings, buses, and trains. Humans are the just natural hosts of variola. Smallpox is not known to be transmitted past insects or animals.
A person with smallpox is sometimes contagious with onset of fever (prodrome phase), merely the person becomes nearly contagious with the onset of rash. At this stage the infected person is usually very ill and not able to move around in the community. The infected person is contagious until the last smallpox scab falls off (CDC, 2004c).
Source: CDC.
The astute clinical symptoms of smallpox resemble other acute viral illnesses, such as influenza, beginning with a 2- to 4-day nonspecific prodrome of fever and myalgias before rash onset. Several clinical features can help clinicians differentiate varicella (chickenpox) from smallpox. The rash of varicella is about prominent on the body and develops in successive groups of lesions over several days, resulting in lesions in various stages of development and resolution. In comparison, the vesicular/pustular rash of smallpox is typically nearly prominent on the face and extremities, and lesions develop at the aforementioned time (CDC, 2001; CDC, 2004c).
The but weapons confronting smallpox are vaccination and patient isolation. Those caring for a patient with smallpox should wear an N95 mask and follow airborne and contact isolation precautions. HEPA filters do remove smallpox virus, but proper procedures must be followed for their effective apply. Vaccination before exposure, or within 3 days later on exposure, affords most complete protection against the illness. Vaccination as late as 4 to 7 days after exposure probable offers some protection from disease or may modify the severity of disease (CDC, 2009a,b).
The smallpox vaccine is made from a virus called vaccinia, which is a pox-type virus related to smallpox. The vaccine contains the live vaccinia virus (other vaccines containing live virus include measles, mumps, and High german measles) and for that reason the vaccination site must be treated carefully to prevent the virus from spreading. The vaccine can accept side effects; all the same, it does not contain the smallpox virus and cannot give you smallpox (CDC, 2009c).
Best Practices for First Receivers
Healthcare workers risk occupational exposures to biological materials when a infirmary receives contaminated patients, particularly during mass casualty events. Hospital employees termed showtime receivers work at a site removed from where the chancy release occurred. This means that their exposures are limited to the substances transported to the hospital on the pare, hair, wearable, or personal effects of the victims. The location and express source of contaminants distinguishes commencement receivers from first responders such every bit firefighters, law enforcement, and ambulance service personnel, who typically respond to the incident site (OSHA, 2005).
Worst-case scenarios have into business relationship challenges associated with communication, resources, and victims. During mass-casualty emergencies, hospitals can anticipate little or no warning before victims brainstorm arriving. Commencement receivers can anticipate that data regarding the hazardous agents may not be available immediately. Hospitals can as well anticipate a large number of self-referred victims (as many every bit 80% of the full number of victims) and should assume victims will not have been decontaminated prior to arriving at the hospital (OSHA, 2005).
An employee's role at a facility and the respective hazards the employee might encounter dictate the level of training that must be provided to whatsoever individual first receiver. Pick of personal protective equipment (PPE) must exist based on a hazard assessment that carefully considers both of these factors, along with the steps taken to minimize the extent of the employee's contact with hazardous substances (OSHA, 2005). Surge chapters, triage, decontamination, security, and disposal of contaminated wastewater must too be addressed.
Surge Capacity
In the upshot of a mass prey issue, healthcare organizations must be able to increase their services quickly in response to the crunch. This is an organization'south surge capacity, "the power to expand care capabilities in response to sudden or prolonged demand" (JCAHO, 2003; Kelen, 2008). Staffing levels, instruction and training, decontamination capabilities, vaccination programs for direct caregivers, volunteer resources, and stockpiling of supplies must be assessed while, in most cases, routine care continues.
Individual personnel on an emergency response team have slightly differing concerns and responsibilities when information technology comes to surge situations. While surge capacity planning is an administrative level concern, individual healthcare providers should understand the basic concept and the need for guidelines in order to participate effectively in training and any necessary implementation. The CDC'southward handbook, Updated In a Moment'due south Notice: Surge Capacity in Terrorist Bombings, and other practiced full general resources are available at this website: http://stacks.cdc.gov/view/cdc/5713/ (CDC, 2010).
The ability of the organization to "degrade gracefully" must also be considered. A healthcare arrangement should have a plan to deal with a reduction in services every bit the number of patients increases. The goal is to engineer and manage failures and thus to avoid "catastrophic failure" (JCAHO, 2003). During a state of emergency, it may be impossible to follow normal do guidelines. The Joint Committee recommends that hospitals and oversight agencies "provide for waiver of regulatory requirements under atmospheric condition of extreme emergency" (JCAHO, 2003).
Triage
Pre-decontamination triage serves three purposes:
- Distinguishes contaminated individuals from other patients arriving at the infirmary past identifying symptoms and victim's proximity to a known chemical release
- Identifies patients who require immediate stabilization before they enter the decontamination system
- Identifies injuries or disquisitional pre-hospital treatment materials that will require special treatment inside the decontamination system (OSHA, 2005)
Post decontamination triage for medical treatment should occur in the infirmary post-decontamination zone afterward victims are inspected and found to exist gratis of contamination. Some hospitals combine decontamination and initial medical treatment (such as antidotes), which ways either the healthcare worker attempts medical triage while wearing PPE (preferred) or the worker is at risk of exposure from victims who have not been adequately decontaminated (OSHA, 2005).
Decontamination Activities
Hospitals must place spaces that volition support decontamination activities (including equipment storage) and ensure that operations tin proceed in the event that one area of the infirmary becomes contaminated. Hospitals planning additions or remodeling projects accept a unique opportunity to blueprint spaces appropriately. Other hospitals should use creative planning to identify existing architectural features that they can use to their advantage. Nonambulatory victims can crave a substantial proportion of first receivers' fourth dimension and efforts, and first receivers are probable to experience the greatest exposure while profitable these victims (OSHA, 2005).
If decontamination is necessary, numerous agencies and organizations recommend a shower time of approximately five minutes for contaminated victims brought to a hospital. Despite the fact that there is no empirical data, operational procedures deem this time to be adequate. Numerous agencies and programs recommend the utilize of h2o and a liquid lather with skilful surfactant properties (such every bit hand dishwashing detergent) to decontaminate victims during emergencies and for mass casualties involving hazardous substances (OSHA, 2005).
Isolation and Lockdown
Hospitals can use a variety of methods to limit unauthorized admission to the emergency section until the victims have been decontaminated. The methods range from a guard at the locked door to sophisticated keycard systems controlled at a central command center. These more than complex systems tend to be associated with urban or recently modernized hospitals and are intended for apply in whatever blazon of disturbance. Hospitals can use these methods if situations suggest that an unruly crowd will force its style into the hospital (OSHA, 2005).
Security
Site security helps maintain order and control traffic effectually the decontamination facility and the hospital entrances. Security officers might need to control a contaminated private to preclude other staff from becoming exposed and to protect equipment. Security officers also ensure contaminated victims practice not bypass the decontamination hospital or enter the ED without passing inspection. In cases of civil disturbance, properly identified security officers protect the decontamination facility and staff so normal operations can continue (OSHA, 2005).
Personal Protective Equipment
Hospitals should select personal protective equipment (PPE) such as respirators, suits, gloves, and confront and center protection based on a hazard assessment that identifies the hazards to which employees might be exposed. Under OSHA'south Personal Protective Equipment Standard, or the parallel Country Plan standards, all employers, including hospitals, must certify in writing that the hazard cess has been performed. For first-receiver PPE, hospitals may base the run a risk cess on OSHA'south Best Practices document. Hospitals likely to respond to incidents involving a specific hazard should adjust the PPE appropriately (OSHA, 2005).
OSHA's Personal Protective Equipment Standard likewise requires that employees be provided with equipment that fits appropriately. Some hospitals assign a set of protective equipment to a specific individual, and that equipment is stored in a container marked with the individual's proper noun. Other hospitals maintain general supplies of PPE, storing sets of equipment by size. In this example, the packages are clearly marked only with the size. Each first receiver tries on equipment in accelerate to make up one's mind what size group fits best so that, during an emergency, the employee can quickly locate an appropriate PPE set (OSHA, 2005).
Personal protective equipment selection for first receivers has been a topic of extensive discussion. At the root of this discussion is the need for hospitals to provide acceptable protection for the reasonably predictable worst-case scenario, despite having express information regarding the nature of the substance with which victims may be contaminated. This lack of information challenges hospitals' abilities to bear the hazard assessments on which PPE pick must be based (OSHA, 2005).
Infection Command
Heightened sensation by infection command (IC) professionals facilitates recognition of the release of a biological agent. Infection control professionals are involved with many aspects of hospital operations and several departments, and with their counterparts in other hospitals. As a upshot, they may recognize changing patterns or clusters in a hospital or in a community that might otherwise go unrecognized (CDC, 2001).
Infection control professionals should ensure that hospitals accept current telephone numbers for notification of both internal and external contacts and that they are distributed to the advisable personnel. They should piece of work with clinical microbiology laboratories, on- or off-site, that receive specimens for testing from their facility to ensure that cultures from suspicious cases are evaluated appropriately (CDC, 2001).
Wastewater Management
Wastewater from decontamination showers can contain depression-level concentrations of the substance(s) with which victims are contaminated. Given the opportunity to plan for decontamination activities (past designing and installing or purchasing decontamination facilities, developing procedures, and preparing staff), hospitals should consider the management of decontamination shower water as part of their emergency preparedness plan (OSHA, 2005).
Decontaminating Surfaces and Equipment
The hospital emergency management plan should include procedures for cleaning equipment and surfaces during and subsequently an incident. Cleaning should be performed past employees who are properly protected and trained. Items that cannot be decontaminated safely should be processed for appropriate disposal. It is unlikely that portable gear could be adequately decontaminated after an incident involving a persistent or highly toxic agent (OSHA, 2005).
Reporting an Incident of Bioterrorism
In the consequence that an incident of bioterrorism occurs in your community, you should know what to report and to whom the report should be sent. First reporters should start at the healthcare organization or hospital level past reporting to the department supervisor, laboratory, and infection control department. Then contact the local wellness/regional departments, which will contact your land's health department and the CDC. Successful reporting of a bioterrorism issue results from good planning, education, and awareness, as well as regular standardized testing earlier an occurrence.
In virtually cases phone will all the same be the principal means for firsthand reporting considering it is direct, rapid, and like shooting fish in a barrel-to-utilize. At that place should ever exist a backup communication plan (eg, cell phones or other ways) in instance of a telephone system failure. In every institution standards should be established to ensure a reliable and immediate response to notifiable diseases and health conditions.
Back Next
Source: https://www.atrainceu.com/content/3-biological-weapons
0 Response to "Which Agents of Bioterrorism Can Be Treated Effectively With Antibiotics? Select All That Apply."
Post a Comment